by Angela Herring
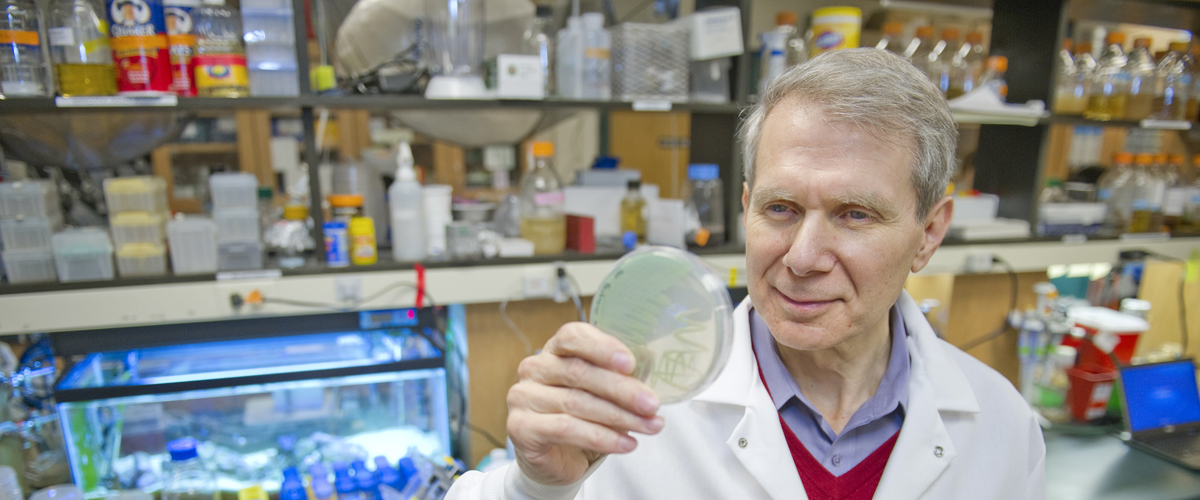
Recent work from University Distinguished Professor of Biology Kim Lewis promises to overcome one of the leading public health threats of our time. In a groundbreaking study published Wednesday in the journal Nature, Lewis’ team presents a novel approach to treat and eliminate methicillin resistant staphylococcus aureus, or MRSA, a potent bacterium whose resistance to antibiotics has kept it one step ahead of researchers. That is, until now.
The so-called “superbug” infects 1 million Americans each year. A major problem with MRSA is the development of deep-seated chronic infections such as osteomyelitis (bone infection), endocarditis (heart infection), or infections of implanted medical devices. Once established, these infections are often incurable, even when appropriate antibiotics are used.
Bacteria such as MRSA have evolved to actively resist certain antibiotics, a fact that has generated significant interest among the scientific and medical communities. But Lewis, Director of Northeastern’s Antimicrobial Discovery Center, suspected that a different adaptive function of bacteria might be the true culprit in making these infections so devastating.
The new work represents the culmination of more than a decade of research on a specialized class of cells produced by all pathogens called persisters. According to Lewis, these cells evolved to survive. “Survival is their only function,” he said. “They don’t do anything else.”
Lewis and his research team posited that if they could kill these expert survivors, perhaps they could cure chronic infections—even those resistant to multiple antibiotics such as MRSA. Furthermore, said Brian Conlon, a postdoctoral researcher in Lewis’ lab and first author on the paper, “if you can eradicate the persisters, there’s less of a chance that resistance will develop at all.”
Lewis, who was elected to the American Academy of Microbiology in 2011 for his scholarship in the field, has found that persisters achieve their singular goal by entering a dormant state that makes them impervious to traditional antibiotics. Since these drugs work by targeting active cellular functions, they are useless against dormant persisters, which aren’t active at all. For this reason, persisters are critical to the success of chronic infections and biofilms, because as soon as a treatment runs its course, their reawakening allows for the infection to establish itself anew.
In the recent study, which also includes contributions from assistant professor Steve Leonard of the Department of Pharmacy Practice, Lewis’ team found that a drug called ADEP effectively wakes up the dormant cells and then initiates a self-destruct mechanism. The approach completely eradicated MRSA cells in a variety of laboratory experiments and, importantly, in a mouse model of chronic MRSA infection.
Coupling ADEP with a traditional antibiotic, Conlon noted, allowed the team to completely destroy the bacterial population without leaving any survivors.
As with all other antibiotics, actively growing bacterial cells will likely develop resistance to ADEP. However, Lewis said, “cells that develop ADEP resistance become rather wimpy.” That is, other traditional drugs such as rifampicin or linezolid work well against ADEP-resistant cells, providing a unique cocktail that not only kills persisters but also eliminates ADEP-resistant mutant bacteria.
Dr. Richard Novick of New York University’s Langone Medical Center and a leader in the field said the research is a “brilliant outgrowth of Kim Lewis’ pioneering work on bacterial persisters and represents a highly creative initiative in this era of diminishing antibiotic utility.”
While ADEP targets MRSA, Lewis’ team believes similar compounds will be useful for treating other infections as well as any other disease model that can only be overcome by eliminating a population of rogue cells, including cancerous tumors. They are pursuing several already.
Originally published in news@Northeastern on November 13, 2013.