by Thea Singer
Reports of the arrival in the U.S. of a new superbug that is resistant to an antibiotic of last resort have set off alarm bells among public health officials.
The new superbug, which was found last month in the urine of a woman from Pennsylvania, is an Escherichia coli bacterium that carries a gene called mcr-1. It has been found to confer resistance to the antibiotic colistin—often the only treatment left for people infected with a lethal family of bacteria known as carbapenem-resistant Enterobacteriaceae, or CRE. Tom Frieden, director of the Centers for Disease Control, has called CRE “nightmare bacteria.”
Fortunately, the Pennsylvania woman’s infection was susceptible to other antibiotics, according to news reports. However, the mcr-1 gene is carried on a circular piece of DNA, or “plasmid,” that can be transferred from one bacterium to another. The great fear is that it could end up in a bacterium that is resistant to all other antibiotics, resulting in a “pan resistant” superbug.
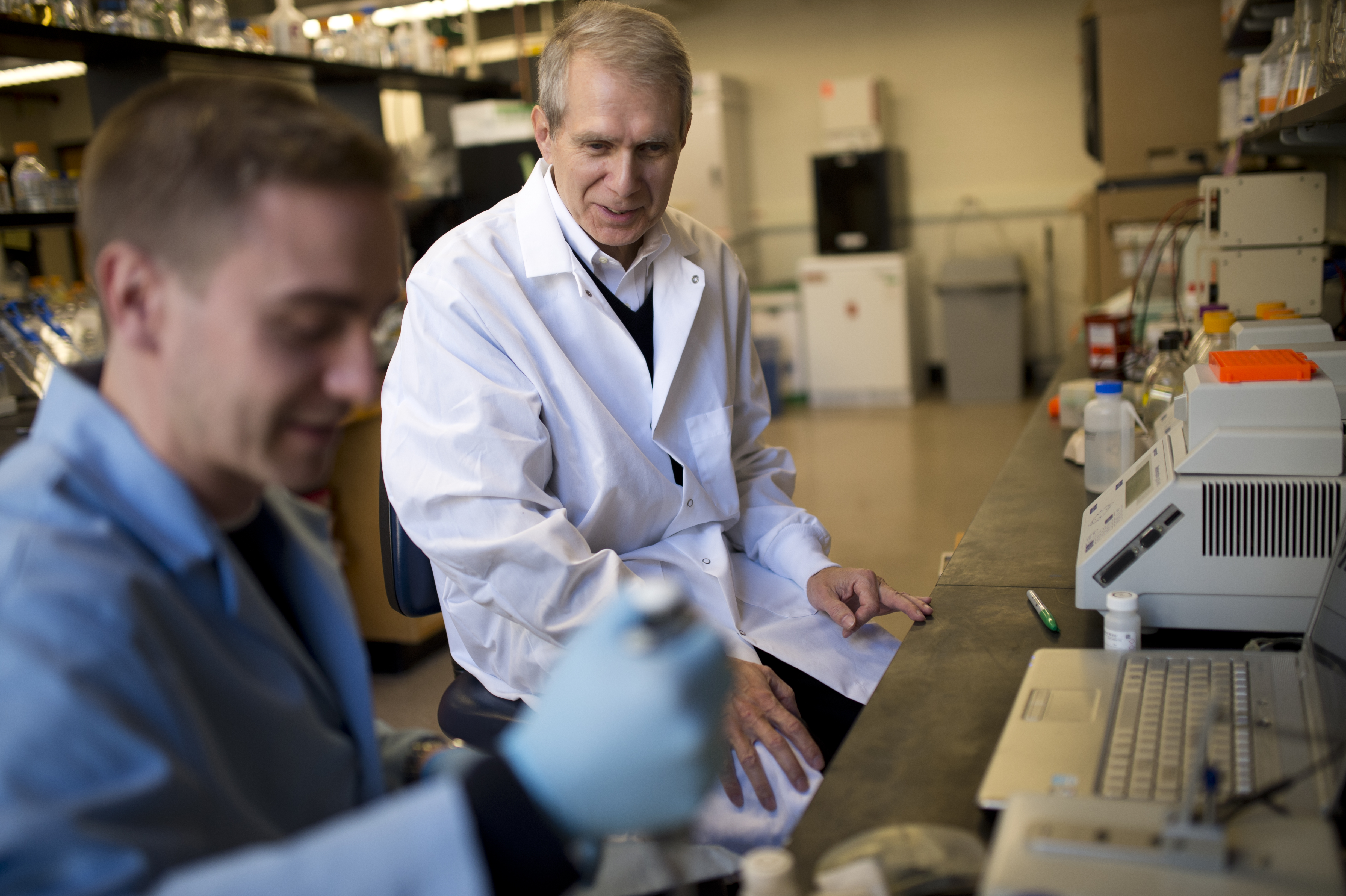
We asked University Distinguished Professor Kim Lewis, who is a leader in the field of antibiotic discovery, to describe the extent of the threat posed by the emergence of mcr-1. Last year a team led by Lewis, who is also the director of Northeastern’s Antimicrobial Discovery Center, discovered the antibiotic teixobactin, which kills bacteria without encountering any detectable resistance. That discovery captured headlines worldwide.
The mcr-1 gene was recently found in E. coli in the U.S. In late 2015 researchers around the world—in China, then Denmark, the Netherlands, France, and Thailand—began reporting that bacteria with the gene were resistant to colistin, a last resort antibiotic. What do these discoveries mean regarding antibiotic resistance overall?
Colistin is a much more important antibiotic than many others. For example, we are one step away from a totally resistant Pseudomonas aeruginosa, one of the tougher bugs to hit that causes life-threatening infections in people with compromised immune systems. Colistin is an antibiotic of last resort for that and it has been very effective. It is an old antibiotic with a high level of toxicity to the kidneys, which is why it had not been used for a while. But with the development of these strains of resistant P. aeruginosa, it became prominent in the arsenal of doctors. Another example is the bacterium Acinetobacter baumannii. Wound infections from resistant strains of A. baumannii emerged in hospitals among soldiers returning from Iraq and Afghanistan, and colistin became the treatment of last resort for them. The saving grace, if you will, of colistin is that resistance to it has heretofore not been easily transmissible. Now with the mcr-1 gene, which is on a plasmid and can hop around from one bacterium to another, that equation has changed.
Bacteria with the mcr-1 gene may be resistant to colistin. But are they resistant to all other antibiotics as well?
That depends. If the gene hops into a bacterium that is resistant to everything else, we have a serious problem. But consider the case of the woman in Pennsylvania: She had a strain of E. coli that did respond to other antibiotics.
Where does teixobactin fit into the picture? Antibiotic resistance occurs when a bacterium acquires a genetic mutation that allows it to code for a protein that no longer binds the antibiotic. Would bacteria with the mcr-1 gene likely be resistant to teixobactin?
Teixobactin inhibits the biosynthesis of two important cell wall “polymers”—sugary molecules needed to build the cell wall. Neither of those polymers are proteins, so they’re not coded directly by genes, which means there’s nothing to mutate. That’s the beauty of teixobactin—it hits immutable targets.
On a big-picture level, teixobactin points us in a new direction. It shows us that we can have antibiotics where development of resistance will be exceedingly unlikely. Our traditional approach to resistance has been trying to introduce antibiotics faster than the bacteria can develop resistance—we’re kind of in a rat race with them. Another, smarter approach is to focus on compounds where the bacteria won’t develop resistance.
Now, teixobactin has its own limitations: It only acts against “gram positive” bacteria. Gram negative bacteria have an additional membrane restricting penetration of most drugs into the cell. E. coli is gram negative, so in that particular case teixobactin would not be helpful. But it would be helpful against an analogous scenario with gram positive bacteria such as methicillin-resistant Staphylococcus aureus (MRSA) or vancomycin-resistant enterococci (VRE), both of which are resistant to almost everything and for which we are running out of options.
Colistin, too, has its limitations, in the other direction: It acts only on gram negative bacteria.
A news article in the December 2015 issue of Nature noted that earlier findings regarding colistin resistance were “concerning” but “they may not be as catastrophic as many media reports have suggested, because colistin is only one of several antibiotics that are rarely used in humans.” Should alarm bells be sounding?
Yes, absolutely. The alarm has been sounded very properly. Consider again the case of P. aeruginosa. With some strains we are only one step away from pan resistance; once they acquire colistin resistance, that’s it.
Originally published in news@Northeastern on June 7, 2016.

Kim Lewis, University Distinguished Professor and Director of the Antimicrobial Discovery Center in the College of Science