In a new type of cancer treatment called immunotherapy, doctors reprogram cells from a patient’s own immune system to fight and kill tumors. The approach has been shown to work in some cases where all other therapies fail. Earlier this month, news broke that a woman with advanced, untreatable breast cancer received immunotherapy treatment and was cured.
The technique is still new and doesn’t currently work for every person or disease. But as doctors continue to hone immunotherapy, Jared Auclair is already thinking about how to get patients in other countries access to the treatment. The key for that to happen lies in the drug approval process.
Here’s how it works: Scientists create a new drug treatment and send an application to every country in the world that requests approval. In the United States, the Food and Drug Administration regulates new drugs. Auclair’s job is to help all the regulatory agencies—the “FDAs around the world”—work in harmony.

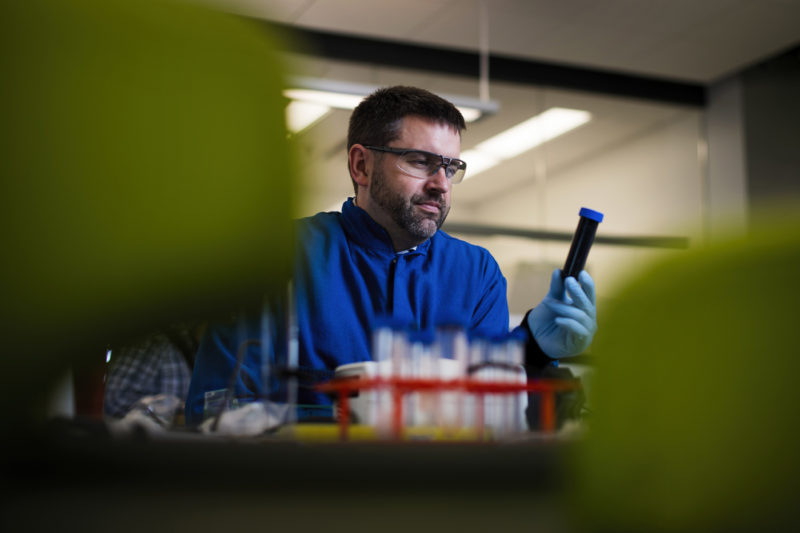
Dr. Jared Auclair Photo by Adam Glanzman/Northeastern University
“Brazil is trying to ensure that drugs stay stable in their humidity, temperature, and climate,” said Auclair, director of executive training and biotechnology programs in the Department of Chemistry and Chemical Biology at Northeastern. “Drugs all act a certain way in different instances, just like meat would.” Drug safety guidelines are specific to each country. For example, the approval process for a new drug will be different in Brazil because its climate is different from that of the United States.
The problem is that approving a new drug with all the country-specific requirements can take months, or even years, and patients need them now. To help bring cutting-edge treatments to market faster, Auclair visits international regulators all over the world and gives them hands-on training. He’s worked with labs from Papua New Guinea, Russia, Chile, and Peru, to name a few. In August, he will travel to Brazil to train the regulatory agency there, and in September he’ll head to China.
The idea is that some regulatory agencies don’t have the expertise or tools needed to understand the science behind how a drug works. This keeps drugs from being approved quickly, or sometimes at all. Auclair’s team answers questions and trains regulators so the review process goes faster.
For example, some low-income countries don’t have mass-spectrometers, which are analytical tools scientists use to see how drug molecules behave under certain conditions. During a training session abroad, Auclair can log in and control the mass spectrometer in his lab. This gives regulators in the country hands-on access to the scientific breakthroughs behind how drugs are developed. “We can eliminate some questions they might have so we can get the product to market faster,” said Auclair, who works at Northeastern’s Biopharmaceutical Analysis Training Laboratory at the university’s Innovation Campus in Burlington, Massachusetts.
This work will be especially important as new immunotherapy drugs are approved, Auclair said. Medical doctors and regulators around the world aren’t trained on how to engineer cells for individually tailored cancer treatment. But they will need to understand the process so drugs can get approved and administered safely and effectively, Auclair said.
“We want to make sure that if we’re taking your cells, enhancing them, and giving them back to you, that we give you yours and not the patient in the bed next to you,” Auclair said. “Medical doctors aren’t trained in that space, and we have to make sure it’s done is a controlled manner.”