by Greg St. Martin
Northeastern University researchers have found that the bacterium that causes Lyme disease forms dormant persister cells, which are known to evade antibiotics. This significant finding, they said, could help explain why it’s so difficult to treat the infection in some patients.
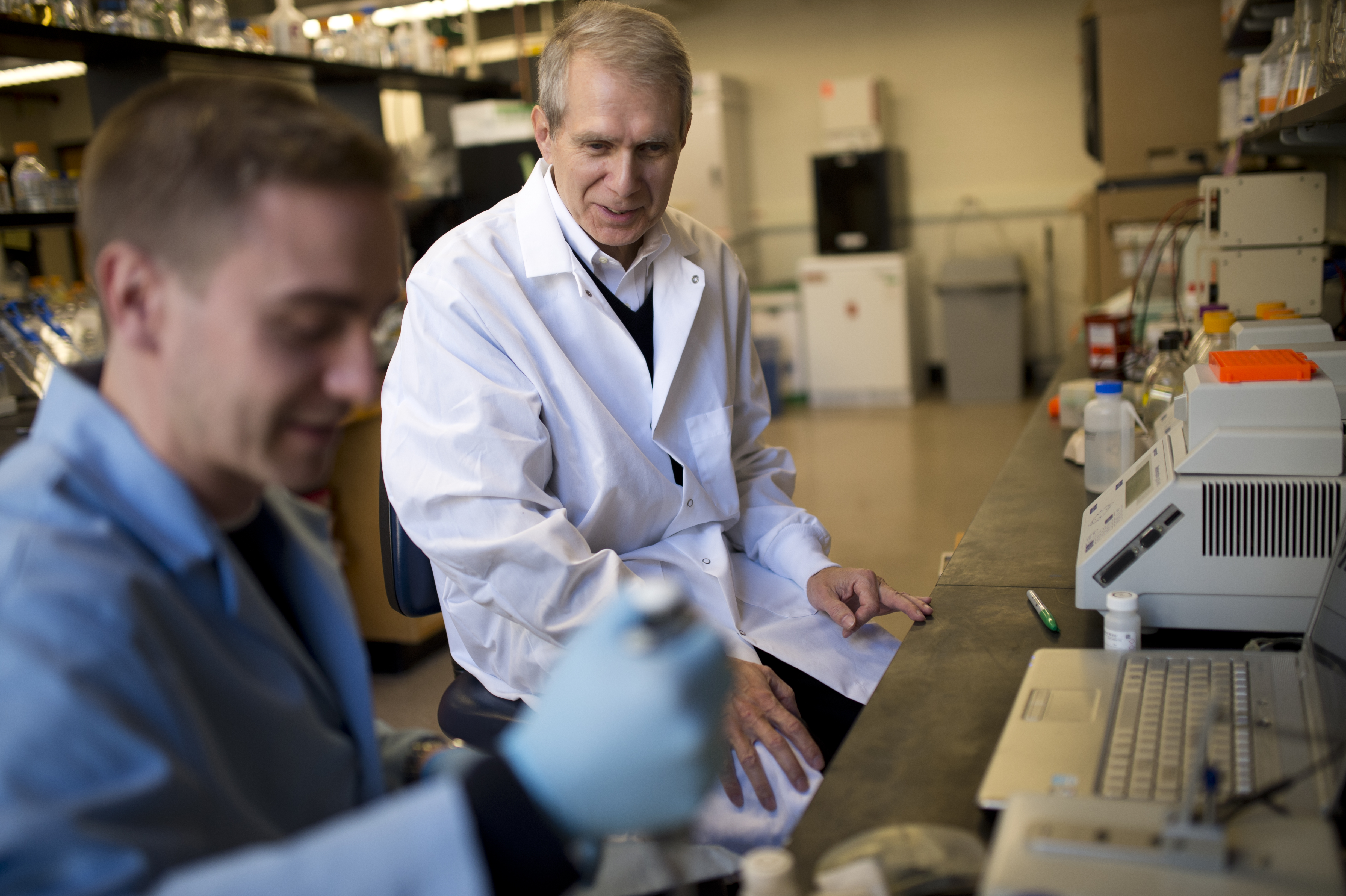
“It hasn’t been entirely clear why it’s difficult to treat the pathogen with antibiotics since there has been no resistance reported for the causative agent of the disease,” explained University Distinguished Professor Kim Lewis, who led the Northeastern research team.
In other chronic infections, Lewis’ lab has tracked the resistance to antibiotic therapy to the presence of persister cells—which are drug-tolerant, dormant variants of regular cells. These persister cells are exactly what they’ve identified here in Borrelia burgdorferi, the bacterium that causes Lyme disease.
The researchers have also reported two approaches—one of them quite promising—to eradicate Lyme disease, as well as potentially other nasty infections.
Lewis and his colleagues presented their findings in a paper published online last week in the journal Antimicrobial Agents and Chemotherapy. He co-authored the paper with Northeastern doctoral students Bijaya Sharma and Autumn Brown, both PhD’16; recent graduate Nicole Matluck, S’15, who received her Bachelor of Science in Behavioral Neuroscience; and Linden T. Hu, a professor of molecular biology and microbiology at Tufts University.
The research was supported by grants from the Lyme Research Alliance and the National Institutes of Health.
Lyme disease affects 300,000 people annually in the U.S., according to the Centers for Disease Control and Prevention, and is transmitted to people via bites from infected blacklegged ticks. If caught early, patients treated with antibiotics usually recover quickly. However, about 10 to 20 percent of patients, particularly those diagnosed later, who have received antibiotic treatment may have persistent and recurring symptoms including arthritis, muscle pain, fatigue, and neurological problems. These patients are diagnosed with Post-treatment Lyme Disease Syndrome.
In addition to identifying the presence of these persister cells, Lewis’ team also presented two methods for wiping out the infection—both of which were successful in lab tests. One involved an anti-cancer agent called Mitomycin C, which completely eradicated all cultures of the bacterium in one fell swoop. However, Lewis stressed that, given Mitomycin C’s toxicity, it isn’t a recommended option for treating Lyme disease, though his team’s findings are useful to helping to better understand the disease.
The second approach, which Lewis noted is much more practical, involved pulse-dosing an antibiotic to eliminate persisters. The researchers introduced the antibiotic a first time, which killed the growing cells but not the dormant persisters. But once the antibiotic washed away, the persisters woke up, and before they had time to restore their population the researchers hit them with the antibiotic again. Four rounds of antibiotic treatments completely eradicated the persisters in a test tube.
“This is the first time, we think, that pulse-dosing has been published as a method for eradicating the population of a pathogen with antibiotics that don’t kill dormant cells,” Lewis said. “The trick to doing this is to allow the dormant cells to wake up.”
He added: “This gives you an idea that you could, in principle, establish a similar regiment for treating patients for this and other chronic diseases.”
Lewis is a faculty member in the biology department and directs Northeastern’s Antimicrobial Discovery Center. Over the past decade he has led pioneering work on this specialized class of cells produced by all pathogens known as persisters. Earlier this year, Lewis, biology professor Slava Epstein, and other colleagues published groundbreaking research in Nature presenting a new antibiotic that kills pathogens without encountering any detectable resistance.
In previous work, Lewis’ lab identified a compound called ADEP that causes dormant persister cells in MRSA to self-destruct. This compound was among the first options the researchers tried out to combat Lyme disease. But it didn’t work, and neither did combinations of standard antibiotics used to treat the disease. The team thought it had hit a dead end yet remained vigilant in its quest to identify promising alternative options.
“What we came up with was the pulse-dosing regimen, which worked beautifully,” Lewis explained. “I think this could be very useful, especially for antibiotics for which resistance doesn’t rapidly develop.”
Though the researchers identified the presence of these persister cells, they also note in their paper that the mechanisms by which the persisters are able to survive remain unknown. More work in this area will be required, they wrote.
Originally published in news@Northeastern on June 1, 2015

University Distinguished Professor Kim Lewis is a faculty member in the biology department and is director of the Antimicrobial Discovery Center at Northeastern. Photo by Brooks Canaday/Northeastern University